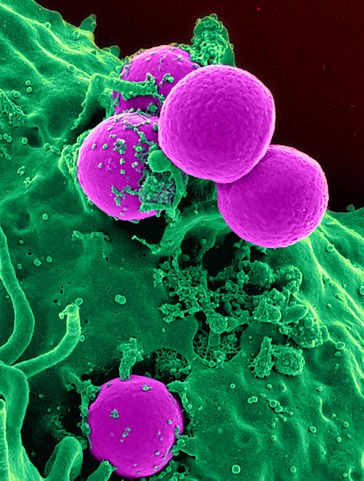
Staphylococcus aureus is a bacterium that is commonly found on the skin and in the nasal passages of healthy individuals. While it is a part of the normal human flora, certain strains of Staphylococcus aureus, especially methicillin-resistant Staphylococcus aureus (MRSA), have gained notoriety for their resilience and ability to cause infections, particularly in healthcare settings. Here’s an exploration of the resilience of Staphylococcus aureus in healthcare settings:
1. Antibiotic Resistance:
- MRSA: Methicillin-resistant Staphylococcus aureus (MRSA) is a strain of Staphylococcus aureus that is resistant to multiple antibiotics, including beta-lactams like methicillin. This resistance complicates treatment and contributes to the bacterium’s persistence in healthcare environments.

2. Biofilm Formation:
- Surface Adherence: Staphylococcus aureus has the ability to adhere to surfaces and form biofilms. Biofilms are communities of bacteria encased in a protective matrix, making them more resistant to antibiotics and disinfectants.
- Medical Devices: Staphylococcus aureus biofilms often form on medical devices such as catheters, implants, and prosthetic devices, increasing the risk of device-related infections.
3. Nasal Colonization:
- Carrier State: Many individuals are carriers of Staphylococcus aureus, particularly in their nasal passages, without showing symptoms of infection. This carrier state can contribute to the spread of the bacterium in healthcare settings.
4. Person-to-Person Transmission:
- Direct Contact: Staphylococcus aureus can be transmitted through direct contact with infected individuals or carriers. In healthcare settings, where close patient contact is common, this can lead to the spread of the bacterium.
5. Environmental Contamination:
- Survival on Surfaces: Staphylococcus aureus can survive on environmental surfaces for extended periods, contributing to the contamination of healthcare environments. Regular cleaning and disinfection are essential to control its spread.
6. Adaptation to Healthcare Practices:
- Selective Pressure: The use of antibiotics and other antimicrobial agents in healthcare settings can exert selective pressure on Staphylococcus aureus, favoring the survival and proliferation of resistant strains.
- Healthcare-Associated Infections: Staphylococcus aureus is a common cause of healthcare-associated infections (HAIs), including surgical site infections, bloodstream infections, and pneumonia.
7. Asymptomatic Carriage:
- Colonization without Symptoms: Many individuals may carry Staphylococcus aureus asymptomatically. While they may not show signs of infection, they can still serve as a reservoir for the bacterium, contributing to its persistence in healthcare settings.
8. Intracellular Survival:
- Ability to Invade Cells: Staphylococcus aureus has the ability to invade and survive within host cells, making it more challenging for the immune system and antibiotics to eliminate the infection completely.
9. Healthcare Worker Colonization:
- Occupational Risk: Healthcare workers may become colonized with Staphylococcus aureus, increasing the risk of transmission to patients. Adherence to strict hygiene practices, including hand hygiene, is crucial to prevent cross-contamination.
Conclusion:
The resilience of Staphylococcus aureus, especially MRSA, in healthcare settings poses significant challenges for infection control and patient safety. Strategies to address its persistence include strict adherence to infection prevention protocols, surveillance for colonization, judicious use of antibiotics, and ongoing research to develop new therapeutic approaches. Staphylococcus aureus remains a critical focus in healthcare-associated infection control efforts globally.